Diabetes Melitus 5 P
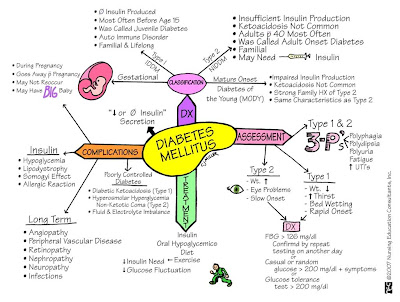
Diabetes mellitus is one of the most common diagnoses made by family physicians. uncontrolled diabetes can lead to blindness, limb amputation, kidney failure, and vascular and heart disease. screening patients before signs and symptoms develop leads to earlier diagnosis and treatment, but may not reduce rates of end-organ damage. randomized trials show that screening for type 2 diabetes does not reduce mortality after 10 years, although some data suggest mortality benefits after 23 to 30 years. lifestyle and pharmacologic interventions decrease progression to diabetes in patients with impaired fasting glucose or impaired glucose tolerance. screening for diabetes melitus 5 p type 1 diabetes is not recommended. the u. s. preventive services task force recommends screening for abnormal blood glucose and type 2 diabetes in adults 40 to 70 years of age who are overweight or obese, and repeating testing every three years if results are normal. individuals at higher risk should be considered for earlier and more frequent screening. the american diabetes association recommends screening for type 2 diabetes annually in patients 45 years and older, or in patients younger than 45 years with major risk factors. the diagnosis can be made with a fasting plasma glucose level of 126 mg per dl or greater; an a1c level of 6. 5% or greater; a random plasma glucose level of 200 mg per dl or greater; or a 75-g two-hour oral glucose tolerance test with a plasma glucose level of 200 mg per dl or greater. results should be confirmed with repeat testing on a subsequent day; however, a single random plasma glucose level of 200 mg per dl or greater with typical signs and symptoms of hyperglycemia likely indicates diabetes. additional testing to determine the etiology of diabetes is not routinely recommended. screening for gdm should be performed using a two-step 50-g nonfasting oral glucose challenge test; if the result is positive, this is followed by a diagnostic 100-g fasting oral glucose tolerance test. 34 further information about screening and diagnosis of gdm is available in a previous article in american family physician (www. aafp. org/afp/2015/0401/p460. html). the diagnosis of diabetes can be made when classic signs and symptoms of hyperglycemia are associated with a single random plasma glucose measurement of 200 mg per dl (11. 1 mmol per l) or greater. alternatively, the diagnosis can be made with an a1c level of 6. 5% or greater, a fasting plasma glucose level of 126 mg per dl (7. 0 mmol per l) or greater, or a two-hour plasma glucose level of 200 mg per dl or greater during an oral glucose tolerance test with 75-g glucose load (table 217); however, testing should be repeated on a subsequent day to confirm the diagnosis. 1,17 if testing results do not match the clinical picture or are inconsistent, repeat testing or testing with another modality may be helpful. 17 [corrected] a1c refers to the percentage of glycosylation of the hemoglobin a1c chain and approximates average blood glucose levels over the previous two to three months from the slow turnover of red blood cells in the body. 40 a1c was first included in the ada guidelines as a diagnostic test for diabetes in 2010. despite efforts to standardize laboratory tests, there are some limitations to a1c testing, and an incomplete correlation between a1c level and average glucose level in certain individuals (table 3 4143). for example, hemolytic anemias and acute blood loss can falsely lower a1c levels, whereas prior splenectomy and aplastic anemias, which increase erythrocyte age, can falsely elevate a1c levels. hemoglobinopathies or hemoglobin variants can result in variable changes in a1c level and may be more prevalent among certain racial and ethnic groups. 4448 point-of-care a1c measurements are not recommended for the diagnosis of diabetes. 2,17 a1c testing should be performed in a laboratory using a method certified by the national glycohemoglobin standardization program and consistent with the diabetes control and complications trial reference assay. the national health and nutrition examination survey data indicate that fasting plasma glucose values may identify as many as one-third more undiagnosed cases of diabetes compared with a1c levels. 2,17,49 fasting plasma glucose measurement should be obtained by a venous blood draw; elevated glucometer or continuous glucose monitor measurements are not considered diagnostic. 17 increasingly, diabetes is being recognized as a spectrum of disorders including type 1 diabetes, type 2 diabetes, gdm, prediabetes, neonatal diabetes, maturity-onset diabetes of youth, and latent autoimmune diabetes in the adult. overlap exists in the underlying etiology of these disorders. 2,5,16,5053 autoimmune markers usually present in patients with type 1 diabetes include autoantibodies to one or more of the following: islet cells, insulin, glutamic acid decarboxylase, insulinoma-associated antigen-2, and zinc transporter (table 417,5053). patients with idiopathic type 1 diabetes have no autoantibodies, and some patients with latent autoimmune diabetes in the adult or type 2 diabetes may have certain autoantibodies present making these tests less specific. 5 despite these concerns, the american association of clinical endocrinologists recommend routine confirmation of type 1 diabetes using autoantibody testing. 16 additional research is required to determine whether further testing to classify the etiology of diabetes improves patient outcomes. in the meantime, additional testing is not routinely recommended. Diabetes mellitus, also known simply as diabetes, involves how your body turns food into energy. learn more about the different types of diabetes mellitus. Diabetesmellitus (dm), commonly known as diabetes, is a group of metabolic disorders characterized by a high blood sugar level over a prolonged period of time. symptoms often include frequent urination, increased thirst, and increased appetite. if left untreated, diabetes can cause many complications. acute complications can include diabetic ketoacidosis, hyperosmolar hyperglycemic state, or. Indication for testing diagnostic criteria; symptomatic patients: symptoms or signs of diabetes; a single random blood glucose level ≥ 200 mg/dl is sufficient for diagnosis. ; alternatively, a pathological fasting plasma glucose (fpg) test, oral glucose tolerance test (ogtt), or hemoglobin a1c (hba1c) test establishes the diagnosis (see table below). if hyperglycemia is high enough to.
Diabetes mellitus: an overview diagnosis and tests.
Diabetes Symptoms And Causes Mayo Clinic
Whats The Difference Between Diabetes Mellitus And Diabetes
Diabetesmellitus causes high blood glucose levels and glucose eventually diabetes melitus 5 p spills into the urine. the glucose spillage causes water loss and thus you have the classic polyuria and polydipsia.

See full list on aafp. org. American diabetes association www. diabetes. org/ academy of nutrition and dietetics www. eatright. org diabetes a-z www. niddk. nih. gov/health-information/diabetes. nativa q'alivio quinua negra sal rosada stevia melitus tocosh harina uña de gato vino de mashua ventas: lunes a viernes : 8:00 am a 5:00 pm » horario de consultas con jorge valera: If you have diabetes, see your doctor regularly. people with high blood sugar levels have a higher risk of dehydration. contact your diabetes melitus 5 p doctor immediately if you develop vomiting or diarrhea and are not able to drink enough fluids. monitor your blood sugar as advised by your health care team. report any significant deviations in blood sugar levels.
Diabetes is diagnosed through blood tests that detect the level of glucose in the blood. 1. fasting plasma glucose (fpg) test. a blood sample is taken in the morning after you fast overnight. a normal fasting blood sugar level is between 70 and 100 milligrams per deciliter (mg/dl). diabetes is diagnosed if the fasting blood sugar level is 126 mg/dl or higher. 2. oral glucose tolerance test (ogtt). your blood sugar is measured two hours after you drink a liquid containing 75 grams of glucose. Diagnosing diabetes how is diabetes diagnosed? diabetes is diagnosed with fasting sugar blood tests or with a1c blood tests, also known as glycated hemoglobin tests. a fasting blood sugar test is performed after you have had nothing to eat or drink for at least eight hours. normal fasting blood sugar is less than 100 mg/dl (5. 6 mmol/l). The prognosis in people with diabetes varies. it depends on how well an individual modifies his or her risk of complications. if blood sugar is not well controlled, it can increase a person's risk of heart attack, stroke, and kidney disease, which can result in premature death. disability due to blindness, amputation, heart disease, stroke, and nerve damage may occur. some people with diabetes become dependent on dialysis treatments because of kidney failure. In a systematic review of 44,203 individuals from 16 cohort studies with diabetes melitus 5 p a follow-up interval averaging 5. 6 years (range 2. 8--12 years), those with an a1c between 5. 5 and 6. 0% had a substantially increased risk of diabetes with 5-year incidences ranging from 9 to 25%.
Jennifer mayfield, m. d. m. p. h. is associate professor of family medicine at bowen research center, indiana university, indianapolis. she received a medical degree from loma linda (calif. ) school of medicine and completed a residency in family medicine at the university of minnesota medical school, minneapolis. dr. mayfield has served as chair of the council on foot care for the american diabetes association for the past two years and was previously the epidemiologist for the indian health service diabetes program. The choice of the new cutoff point for fasting plasma glucose levels is based on strong evidence from a number of populations linking the risk of various complications to the glycemic status of the patient. figure 1 shows the risk of diabetic retinopathy based on the glycemic status of 40to 74-year-old participants in the national health and nutritional epidemiologic survey (nhanes iii). 2 the risk of retinopathy greatly increases when the patient's fasting plasma glucose level is higher than 109 to 116 mg per dl (6. 05 to 6. 45 mmol per l) or when the result of a 2hrppg test is higher than 150 to 180 mg per dl (8. 3 to 10. 0 mmol per l). however, the committee decided to maintain the cutoff point for the 2hrppg test at 200 mg per dl (11. 1 mmol per l) because so much literature has already been published using this criterion. they selected a cutoff point for fasting plasma glucose of 126 mg per dl (7. 0 mmol per l) or higher. this point corresponded best with the 2hrppg level of 200 mg per dl (11. 1 mmol per l). the risk of other complications also increases dramatically at the same cutoff points. a normal fasting plasma glucose level is less than 110 mg per dl (6. 1 mmol per l) and normal 2hrppg levels are less than 140 mg per dl (7. 75 mmol per l). blood glucose levels above the normal level but below the criterion established for diabetes mellitus indicate impaired glucose homeostasis. persons with fasting plasma glucose levels ranging from 110 to 126 mg per dl (6. 1 to 7. 0 mmol per l) are said to have impaired fasting glucose, while those with a 2hrppg level between 140 mg per dl (7. 75 mmol per l) and 200 mg per dl (11. 1 mmol per l) are said to have impaired glucose tolerance. both impaired fasting glucose and impaired glucose tolerance are associated with an increased risk of developing type 2 diabetes mellitus. lifestyle changes, such as weight loss and exercise, are warranted in these patients. Diabetes mellitus causes high blood glucose levels and glucose eventually spills into the urine. the glucose spillage causes water loss and thus you have the classic polyuria and polydipsia. the. The new classification system identifies four types of diabetes mellitus: type 1, type 2, other specific types and gestational diabetes. arabic numerals are specifically used in the new system to minimize the occasional confusion of type ii as the number 11. each of the types of diabetes mellitus identified extends across a clinical continuum of hyperglycemia and insulin requirements. type 1 diabetes mellitus (formerly called type i, iddm or juvenile diabetes) is characterized by beta cell destruction caused by an autoimmune process, usually leading to absolute insulin deficiency. 2,7 the onset is usually acute, developing over a period of a few days to weeks. over 95 percent of persons with type 1 diabetes mellitus develop the disease before the age of 25, with an equal incidence in both sexes and an increased prevalence in the white population. a family history of type 1 diabetes mellitus, gluten enteropathy (celiac disease) or other endocrine disease is often found. most of these patients have the immune-mediated form of type 1 diabetes mellitus with islet cell antibodies and often have other autoimmune disorders such as hashimoto's thyroiditis, addison's disease, vitiligo or pernicious anemia. a few patients, usually those of african or asian origin, have no antibodies but have a similar clinical presentation; consequently, they are included in this classification and their disease is called the idiopathic form of type 1 diabetes mellitus. 2,7 types of diabetes mellitus of various known etiologies are grouped together to form the classification called other specific types. this group includes persons with genetic defects of beta-cell function (this type of diabetes was formerly called mody or maturity-onset diabetes in youth) or with defects of insulin action; persons with diseases of the exocrine pancreas, such as pancreatitis or cystic fibrosis; persons with dysfunction associated with other endocrinopathies (e. g. acromegaly); and persons with pancreatic dysfunction caused by drugs, chemicals or infections. 2,7 the etiologic classifications of diabetes mellitus are listed in table 1. 2 the definition and diagnosis of gestational diabetes mellitus was not altered in these new recommendations. 2 gestational diabetes mellitus is an operational classification (rather than a pathophysiologic condition) identifying women who develop diabetes mellitus during gestation. 7 (women with diabetes mellitus before pregnancy are said to have pregestational diabetes and are not included in this group. ) women who develop type 1 diabetes mellitus during pregnancy and women with undiagnosed asymptomatic type 2 diabetes mellitus that is discovered during pregnancy are classified with gestational diabetes mellitus. however, most women classified with gestational diabetes mellitus have normal glucose homeostasis during the first half of the pregnancy and develop a relative insulin deficiency during the last half of the pregnancy, leading to hyperglycemia. the hyperglycemia resolves in most women after delivery but places them at increased risk of developing type 2 diabetes mellitus later in life.
The expert committee recommended that screening for gestational diabetes mellitus be reserved for use in women who meet one or more of the following criteria: 25 years of age or older, obese (defined as more than 120 percent above their desirable body weight), a family history of a first-degree relative with diabetes mellitus, and belong to a high-risk ethnic population. See full list on drugs. com. Introduction. diabetes mellitus (dm), which is related to cardiovascular disease, is one of the main global health problems. in ethiopia, information about this disease is known to be scarce. objective. to assess the prevalence of diabetes mellitus and its risk factors among individuals aged 15 years and above. methods. a community-based cross sectional study was carried out from january 01.

1. american diabetes association. diagnosis and classification of diabetes mellitus. diabetes care. 2004;27(suppl 1):s5s10. Type 1 diabetes cannot be prevented. you can decrease your risk of developing type 2 diabetes. if a close relative—particularly, a parent or sibling—has type 2 diabetes, or if your blood glucose test shows \\"pre-diabetes\\" (defined as blood glucose levels between 100 and 125 mg/dl), you are at increased diabetes melitus 5 p risk for developing type 2 diabetes. you can help to prevent type 2 diabetes by 1. maintaining your ideal body weight. 2. exercising regularly—such as a brisk walk of 1-2 miles in 30 minutes—at le Diabetes initially might not cause any symptoms. it can sometimes be caught early with a routine blood test before a person develops symptoms. when diabetes does cause symptoms, they may include: 1. excessive urination 2. excessive thirst, leading to drinking a lot of fluid 3. weight loss. people with diabetes also have an increased susceptibility to infections, especially yeast (candida) infections. when the amount of insulin in the blood stream is too low, extremely high blood sugar levels c Jun 27, 2019 · diabetes mellitus (dm) is a group of metabolic disorders that cause sustained high blood sugar levels. in the past, only two types of diabetes were known, type 1 and type 2.
Comments
Post a Comment